A new era in mental health care and research
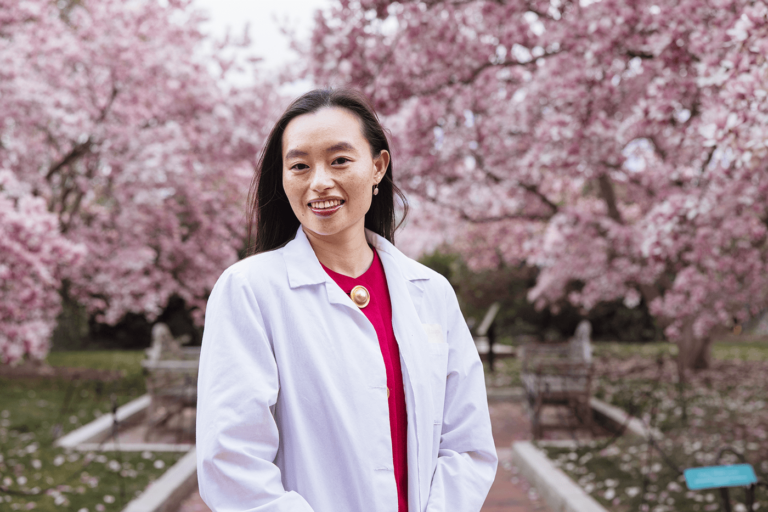
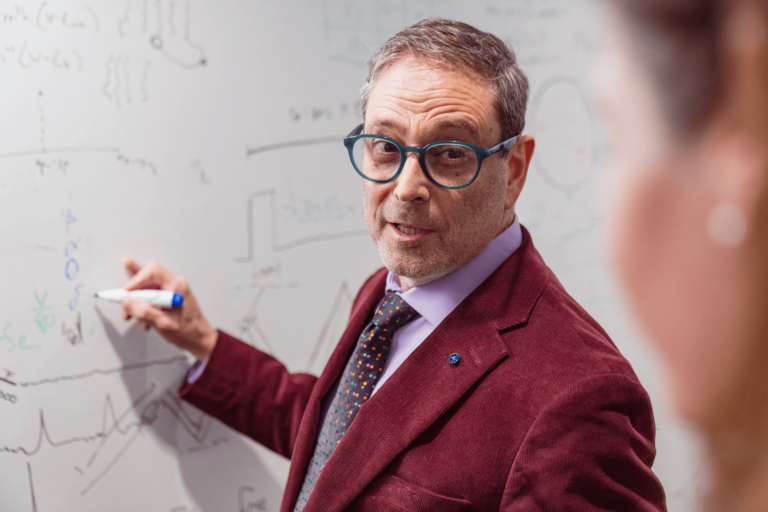
Eric Lenze, BA ’90, MD ’94
By Julie Leistner
Eric Lenze, BA ’90, MD ’94, leads the Department of Psychiatry at WashU Medicine, which has a long history of international excellence in research, education, and patient care. Lenze’s clinical work focuses on treating depression, anxiety, and cognitive disorders in older adults. His research has advanced evidence-based medicine in these areas of care, particularly treatment-resistant depression. During the COVID-19 pandemic, he achieved international distinction by showing that the psychiatric drug fluvoxamine was an effective treatment for COVID-19 — an exciting example of drug repurposing. He directs the Healthy Mind Lab, whose research promotes mental and physical health across the lifespan. Lenze also co-directs the Center for Perioperative Mental Health, which addresses older adults’ mental health needs related to surgery. He joined the WashU faculty in 2007 and became department head in 2022.
What makes the Department of Psychiatry at WashU Medicine special?
WashU brought the field of psychiatry into modern medicine. It used to be commonplace to blame patients and their families for their mental illness; it was thought of as a moral failing. Our department changed that by approaching psychiatric conditions like depression, autism, and schizophrenia in terms of biology and genetics. That perspective changed the entire field for the better. Today, we have effective treatments, and there is much less stigma around mental illness.
“Scientists here are eager to work together, because we know that’s the best way to make big leaps in discovery. Fort Labs allows us to do that.”
Eric Lenze, Wallace and Lucille K. Renard Professor of Psychiatry Head, Department of Psychiatry at
WashU Medicine
Another thing that sets us apart is that we are an integral part of a world-beating neuroscience research community here at WashU. So, as we in the Department of Psychiatry study mental health, we collaborate with experts from every related field imaginable: genetics, imaging, anesthesiology, neuroscience, neurology, drug discovery — you name it. This kind of cross-discipline collaboration doesn’t happen everywhere, but it’s routine at WashU. By working together in this way, we can spot important biological connections we might otherwise miss, and we move our discoveries forward quickly.
Why is psychiatric research so important?
About one out of every four or five people in this country suffers from a mental illness. That means that in every family, there’s someone either dealing with mental illness or soon to be dealing with mental illness. It affects all of us, one way or the other.
We still don’t have a good understanding of the biological foundations of mental disorders, much the way cancer was 40 years ago. In our department, neuroscientists are trying to pick that apart, literally cell by cell. We are building an understanding of how processes at the tiniest molecular level ultimately lead to illnesses such as depression, schizophrenia, and bipolar disorder.
The good news is that we’re making important discoveries every day. We’re really at the precipice of breakthroughs that are going to transform how mental illness is treated.
How is the Jeffrey T. Fort Neuroscience Research Building, or Fort Labs, supporting that progress?
WashU is home to one of the largest neuroscience research hubs in the world, with more than 100 research teams. Fort Labs brings them all together in one place. It is the largest neuroscience research building in the country. It’s designed to foster what we call the secret sauce at WashU, and that’s the cross-discipline collaboration I mentioned earlier. Scientists here are eager to work together, because we know that’s the best way to make big leaps in discovery. Fort Labs allows us to do that.

Can you tell us more about the power of collaboration?
At Fort Labs, we have people studying different kinds of disorders ranging from Alzheimer’s disease to chronic pain, to of course, mental disorders like depression. Most people might think of these conditions as being separate. But we now know that they actually share a lot in common. There are developments in neurology and anesthesia right now that are helping us develop new ways to treat psychiatric disorders. We expect that many of our discoveries will apply broadly across many disease areas. That’s how you have a big impact.
If you could change one thing in the world, what would it be?
I would offer people with mental disorders and their families new hope. These tend to be chronic conditions that often strike people early in their lives. Frequently, our system doesn’t have good answers for them, and so their families go on a long and difficult journey to try to get treatment. And I want us to be there for them, developing effective new therapies and offering outstanding care for people in all walks of life.
I see fantastic new discoveries at WashU literally every day. Our work is going to change how psychiatry is practiced generations from now. It’s an exciting time.
From WashU to DARPA
In her first year of high school, Alissa Ling, AB ’18, started volunteering more than 10 hours a week at Walter Reed Military Medical Center. There, she first learned about emerging rehabilitation devices — like brain-controlled prosthetic arms — that offered soldier amputees a rare and vital return to mobility.
Expert hands, timely hope
WashU Medicine’s Taylor Family Department of Neurosurgery is home to the latest innovations in neurosurgery and neurotechnology to address complex brain tumors. Eric C. Leuthardt, MD, performed a groundbreaking, minimally invasive procedure in 2010.
The healing power of neuroscience
Physician-scientist Michael Avidan, MBBCh, leads WashU Medicine’s Department of Anesthesiology, a world leader in anesthesiology research, education, and patient care.